Infectious Diseases Case of the Month #9 |
|||
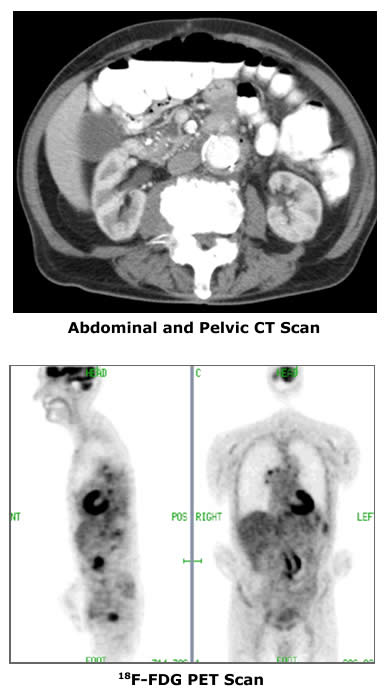 |
An 88 y.o. white male was admitted to the hospital in August 2006 with recurrent fevers and rigors. A resident of Virginia the patient was visiting relatives in Michigan when he abruptly became ill while attending a baseball game. Within a short time of his admission to the hospital he was found to be bacteremic with multiple cultures positive for Methicillin Resistant Staphylococcus aureus. Previously, beginning in the spring of 2006, he had had a series of poorly explained bacteremic illnesses. These included Klebsiella bacteremia in March 2006, coincident Klebsiella and group A streptococcal bacteremias in May 2006, and coincident MRSA and Klebsiella bacteremias in June 2006. Workup including trans-esophageal echocardiography, WBC scan, and abdominal and pelvic CT scans did not reveal an origin of his problem. Each time the patient was treated with courses of prolonged appropriate antibiotic therapy and appeared to improve.The patient's past medical history was notable for coronary artery disease, peripheral vascular disease, and anemia that had previously required blood transfusion. In Aug 2000 he had undergone an Ancure aortic endograft repair of an infrarenal abdominal aortic aneurysm. Subsequent enlargement of the aneurysm was determined to be due to a Type 1 endoleak and necessitated open repair of the endograft in March 2002. He underwent colonoscopic polypectomy in the fall of 2005. On examination the patient did not have focal localizing signs or symptoms. A systolic ejection murmur was noted. Initial laboratory data included WBC 21.4 (H) and Hgb 9.9 (L). LFT's and pancreatic enzymes were normal. An abdominal CT scan showed a 3.7 x 2.5 cm cystic mass in the head of the pancreas that may have been chronic. An additional image from that CT Scan is pictured at upper left. A trans-esophageal echocardiogram did not suggest the presence of valvular vegetations, and a labeled WBC scan was again negative (as it had been in Virginia). The patient's bacteremia persisted for four days despite therapy with Vancomycin. He began to feel better only to suffer a relapse a week after admission at which time he was then found to be bacteremic with Klebsiella oxytoca. Because the origin of the patient's bacteremias remained uncertain, a PET scan was performed. PET Scan images are pictured at lower left. |
||
What is the most likely source of this man's recurrent bacteremias? Click here for the answer. |
|||
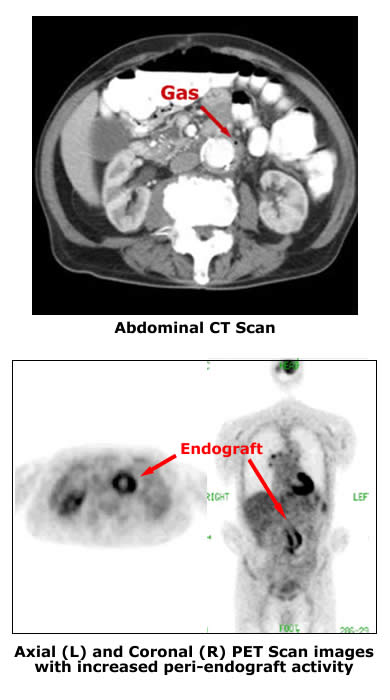 |
This patient had an infected aortic endograft with erosion into adjacent bowel. 18F-FDG PET scanning aided in the diagnosis. Trans-femoral, percutaneous stent-grafting (endografting) has assumed an increasing role in repair of infarenal aortic aneurysms. Reported advantages include decreased peri-operative morbidity and mortality. Rates of infection of percutaneously placed aortic endografts are unknown. Diagnosis of vascular graft infections (including those of endoprostheses/endografts) can be quite difficult. Typically this is attempted with imaging studies including CT scans and labeled WBC scans. Clues to the presence of infection can include peri-graft fluid and the accumulation of labeled WBC's in the vicinity of the graft. In the case described endograft infection was suspected. The presence of a small gas bubble adjacent the endograft seen on CT scan (see image at upper left) and the recurrent nature of the bacteremias was suggestive of endovascular infection. The varied nature of the microbiology was peculiar and did raise some concern for a communication with the gi tract. Definitive surgical treatment of an infected aortic endograft is complex and is associated with substantial morbidity and mortality. Therefore it was desired to have the most definitive diagnosis possible in this case. PET scanning was employed for this purpose and showed local abnormal tracer accumulation in the vicinity of the endograft (see image at lower left) suggesting this was the likely infectious source. Fluorodeoxyglucose (FDG) Positron Emission Tomography (PET) radionuclide imaging is indicated in the evaluation of a number of malignancies. It has potential applications in the diagnosis of infectious diseases as well, but this use is not yet generally reimbursed by government and commercial payors. Labeled FDG is taken up by metabolically active cells including inflammatory cells and thus providing the basis for its potential utility in diagnosis of infectious diseases. Compared to other nuclear medicine modalities useful in the diagnosis of infectious diseases PET scanning is said to have advantages of speed, spatial resolution, and higher quality images. Its potential drawback is in specificity which can be partially compensated for by "fusion" technology of FDG-PET and CT. At the request of family this patient was transferred to a tertiary facility. There he underwent graft resection and extra-anatomic bypass. He was indeed found to have infection adjacent the endograft and with communication to adjacent bowel. Unfortunately, he died of a cardiac event sometime after surgery. Ref: Fukuchi, K. et al, Detection of aortic graft infection by fluorodeoxyglucose positron emission tomography: Comparison with computed tomographic findings, Jr of Vasc Surg, 42:5, 919-925, 2005. |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||