Infectious Diseases Case of the Month Case #35 |
|||
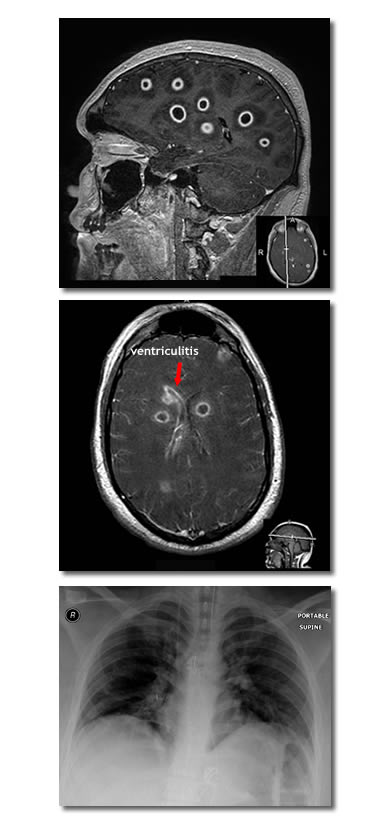 |
A nineteen year old white male was admitted to the hospital for meningitis. Previously healthy, he had not been feeling well for several days with complaints of headache, neck pain, and right shoulder pain. He developed confusion which prompted family members to bring him to the emergency room for medical attention. In the emergency room he was noted to have fever (100.2o) and to have a stiff neck. A lumbar puncture was performed (described as "traumatic" with only 2 cc of spinal fluid obtained) with the following results: WBC 4220 (67% PMN's, 27% monos), RBC 60, Glu 31 mg/dl, and protein 397 mg/dl. Gram stain of the CSF showed many PMN's but no organisms were seen. The patient was begun on IV vancomycin and ceftriaxone. He required endotracheal intubation because of progressive obtundation. A CT scan (not pictured) showed extensive but vague areas of hypoattenuation bilaterally in the cerebral hemispheres, the basal gangila, and the thalami. To further evaluate, an MRI scan was obtained which showed a dramatic picture of widely distributed ring enhancing lesions (two representative images are at left). The patient was estimated to have at least thirty to thirty-five of these fairly uniformly sized lesions and had evidence of right lateral ventriculitis. Also evident on neuro-imaging was sphenoid sinusitis without boney erosion (not pictured). Click here for larger views of the sagittal MRI image and the patient's CXR (bottom image at left). The patient was a native of Oregon and resided on the Oregon Coast. Approximately three months before the onset of his illness he had worked in a fish cannery where hake was processed. He had not directly handled the fish but had been involved in the final packaging process for shipment. Many co-workers were foreign born including many from Latin America. He was not an outdoorsman and specifically had not swam recently in freshwater. Family members were unaware of any HIV risks. The patient remained obtunded. Blood cultures and the initial CSF culture were negative. HIV antibody was negative. A transesophageal echocardiogram was negative for valvular vegetations or evident intra-cardiac shunt. He developed a rash and bronchospasm thought perhaps related to ceftriaxone. Meropenem was substituted. Multiple serologies and a repeat lumbar puncture were performed. Neurosurgeons were consulted but did not favor immediate brain biopsy for fear of low diagnostic yield and potential hazards to this young individual. Of the choices below what the likely the cause of this illness? |
||
What was the likely cause of this illness? |
|||
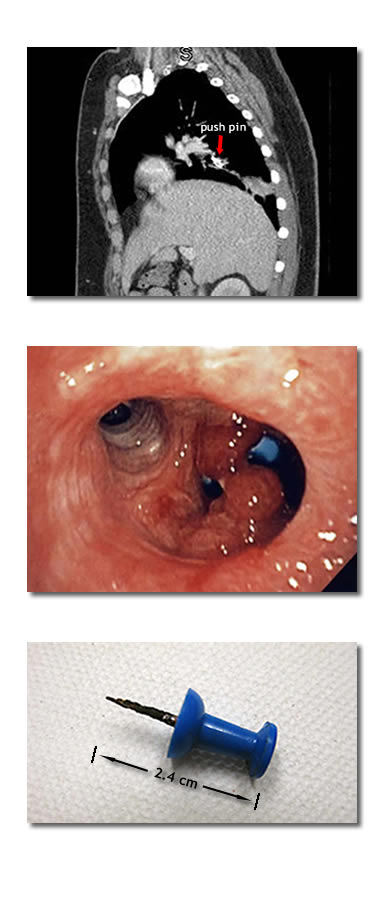 |
Cultures of a second CSF specimen obtained on the third hospital day (and after 2-3 days of IV antibiotics) grew Streptococcus intermedius. At the request of the ID physician the second CSF specimen had been inoculated into more enriched (blood culture) media than was the original specimen, and the organism grew after prolonged incubation. CSF cultures for fungi and AFB were negative. Serologies for cysticercosis, toxoplasmosis, and Entamoeba histolytica were negative. CSF cryptococcal antigen, urine pneumococcal antigen, and Quantiferon Gold tests were negative. Given the prior antibiotics it is possible that the brain abscesses may indeed have included other organisms in addition to Streptococcus intermedius. Indeed, one could question whether Streptococcus intermedius was itself a true pathogen here given the inability to isolate it in either initial blood or CSF specimens. However, given this organism's well described ability to cause pyogenic abscess and the fact that the patient did eventually respond to antimicrobial therapy directed at bacterial pathogens, it is very likely this indeed was a significant pathogen. Streptococcus intermedius is one of the Streptococcus anginosus group of viridans streptococci and as mentioned above, is well known for a propensity to cause pyogenic abscess. Indeed, anginosus group streptococci have a strikingly prominent association with brain abscess being isolated in approximately 50-80% of such cases. They are much less common causes of meningitis. Meningits in this case could even have resulted from rupture of one or more of the many abscesses into the meningeal or ventricular spaces. The origin of these dramatically widespread abscesses was not defined with absolute certainty. Sphenoid sinusitis was one possible origin but seems unlikely as the abscesses were not localized to portions of the brain adjacent the sphenoid but instead had a distribution more consistent with hematogenous origin (the patient nonetheless did undergo endoscopic drainage of the sphenoid sinus). Eventually, CT scans of the chest, abdomen, and pelvis were performed seeking a possible source of the brain abscesses. Unexpectedly, on the chest CT (see image topmost at left) there was noted a foreign body with associated infiltrate. In retrospect this foreign body had also been evident on single view chest x-rays (see Chest X-ray). When the patient had recovered sufficiently to provide history, he related the fact that indeed he recalled "swallowing" a push pin perhaps two years earlier. Pictured at left are bronchoscopic photos of this embedded foreign body (middle image) and its appearance after successful extraction (lowermost image). Brain abscesses associated with pulmonary foreign bodies have been described in the pediatric medical literature. Indeed, in the absence of another convincing cause of these apparently hematogenously distributed abscesses, chronic infection associated with this foreign body may have been the most likely origin of this patient's illness. Although drainage as well as antibiotic therapy is ideal treatment for brain abscess, the multiple lesions made this approach impractical. Instead the patient was treated with prolonged IV antibiotics and has appeared to do well. Ref: Roberts, J. et al, Airway foreign bodies and brain abscesses: Report of two cases and review of the literature, Int J Pediatr Otorhi, 72:2, pgs. 265-269, 2008 |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||