Infectious Diseases Case of the Month Case #30 |
|||
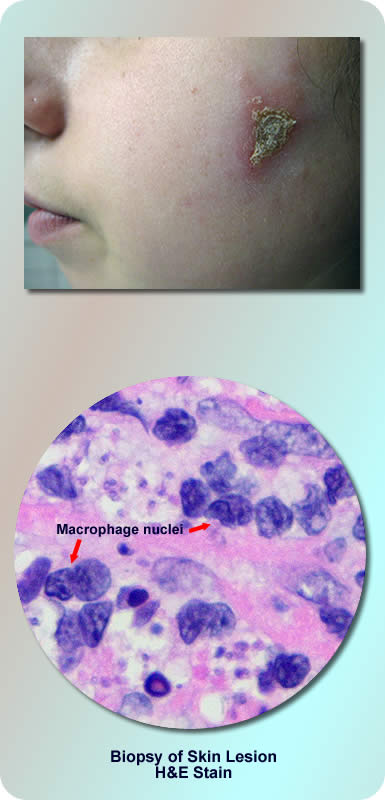 |
A 21 year old female was seen in infectious diseases clinic for persistent non-healing bilateral facial and right neck sores. She was seen about two months after she had returned from a two month stay in Costa Rica where she had worked on as a volunteer assisting local "organic" farmers. The facial lesions had first appeared approximately one month into her two month stay in Costa Rica. One of the facial lesions is pictured at upper left. She had found the sores sometimes uncomfortable but otherwise she had felt well. She had had no fevers, chills, or other constitutional symptoms. Topical antibiotic cream, two courses of TMP/SMX, and application of triamcinolone cream had not appeared to provide significant benefit. In Costa Rica she had spent her days working in small "sustainable" agricultural settings where she assisted local farmers in the cultivation of a variety of fruits and vegetables. Because of concern about possible exposure to dengue fever, she wore protective clothing and made liberal use of insect repellents while working on the agricultural plots. Indeed, she recalled there were a great many flying insects of different varieties. At night she slept in quarters provided by the host farmers. She erected mosquito netting to protect herself from insect exposure. Prior to her visit to the infectious diseases clinic she had had a biopsy performed of her right neck lesion. A photomicrograph of this biopsy is pictured at lower left. |
||
What was the likely cause of this patient's skin lesions? |
|||
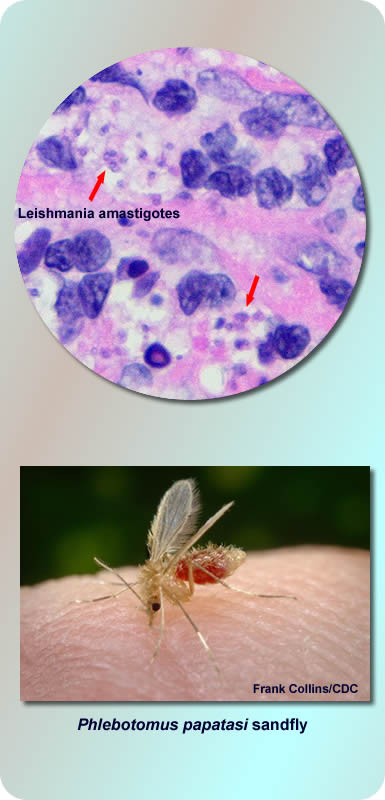 |
This patient had leishmaniasis due to Leishmania panamensis. The biopsy (upper left) had shown histiocytic (macrophage) intracytoplasmic inclusions, the amastigotes of leishmania. Further biopsies were obtained and sent to the CDC for culture where the species Leishmania panamensis was identified by molecular techniques.Leishmaniasis is caused by up to 21 species of leishmania protozoan parasites, transmitted to humans by at least thirty species of sandflies. After leishmania promastigotes are injected by the bite of an infected sandfly, they are phagocytosed by macrophages (see life cycle). It is this parasitization (local or generalized) of the mononuclear phagocyte system that leads to clinical illness. Illness due to leishmania varies depending upon species, geographical acquisition of illness, and innate human immune response. Illness can be cutaneous, mucosal, or visceral depending upon species. Syndromes related to the latter two forms of illness can be potentially disfiguring or fatal respectively. Evaluation of infected patients by clinicians not familiar with leishmaniasis can be baffling given the complexities of species, geographical specificity, and innumerable clinical syndromes. Click here for "key facts" about this extremely complex topic. Leishmania in Costa Rica is predominantly due to Leishmania panamensis (CDC - personal communication). Untreated, the skin lesions typically resolve spontaneously but very slowly (months to years) and leave residual scars. This species like other species of the Vianna subgenus (L. braziliensis, L. guyanensis) can cause the dreaded sequelum of mucosal leishmaniasis where organisms disseminate either hematogenously or via lymphatics to the naso-oropharyngeal mucosa. Mucosal leishmaniasis typically manifests within several years of resolution of the original cutaneous lesions. The incidence of this complication is estimated to be perhaps 5% in persons infected with these species of leishmania. In part because of the potential for mucosal disease, persons infected with Leishmania panamensis are often treated with anti-parasitic therapy. The ideal therapy has not been established. Agents with significant activity include pentavalent antimony compounds (stibogluconate sodium), amphotericin B, pentamidine, and ketoconazole. Most of the other organisms listed as diagnostic choices in the preceding vignette can also cause cutaneous lesions, sometimes not dissimilar in appearance to those of leishmania. Paracoccidioides brasiliensis is a fungus endemic in regions of Central and South America. Mycobacterium leprae can cause anesthetic cutaneous plaques. Fonsecaea pedrosoi, the most common agent of chromoblastomycosis, tends to cause skin lesions of the lower extremities. Although Histoplasmosis capsulatum is less apt to cause skin lesions, it is quite cosmopolitan in its geographic distribution. On biopsy specimens it can appear similar to leishmaniasis. Ref: Herwaldt, B., Leishmaniasis, The Lancet, Vol 354, Oct 2, 1999, pgs 1191-1198. |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||