Infectious Diseases Case of the Month #11 |
|||
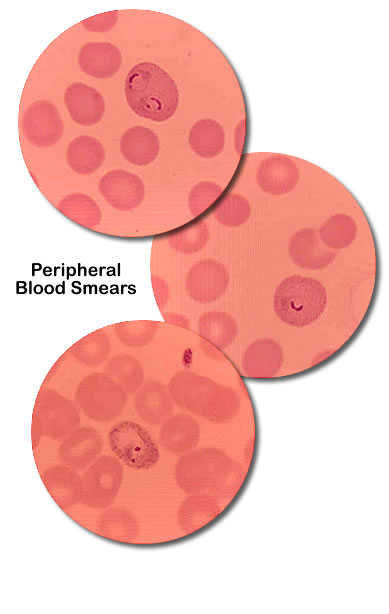 |
A 31 y.o. white male was admitted to the hospital on Christmas Day, 2001 for nausea, vomiting, fever, arthralgias, and severe headache. Normally in good health he had returned from a two week honeymoon trip to the Cook Islands (Rarotonga and Aitutaki) three weeks previously. He had first become ill seven to ten days after his return similarly with shaking chills, nausea, vomiting, arthralgias, and headache. After abating similar symptoms recurred one other time prior to his eventual emergency room presentation. Labs obtained at an outpatient visit a week before admission included WBC 3.9(L), Hbg 15.6, and Plts 45(L). Two years previously the patient had spent a month in Malawi, East Africa visiting his future wife who at that time was a Peace Corps volunteer. He recalled having unpleasant side effects from taking prophylactic anti-malarial medications at the time. It was partly for that reason that he and his fiance chose to honeymoon in the Cook Islands, said to be malaria free by the CDC and WHO. The patient and his new wife stayed at "four star" accommodations and took no particular precautions in regard their food, beverage, or activities. Their visit to the islands was made even more notable by the occurrence of Tropical Cyclone "Trina" which struck the islands during their visit. The patient recalled several mosquito bites. Prior to his travel he had often enjoyed hiking in the Cascade Mountains of western Washington. He was unaware of any recent tick bites.On examination in the emergency room he appeared uncomfortable and complained particularly of headache. Vital signs included temp 102.7, pulse 120, BP 108/38. Laboratory evaluation included: WBC 7.6, Hgb 13(L), Plts 83(L). A lumbar puncture was performed with results including WBC 16 (80% mononuclear cells), glucose 66, protein 50. The patient exhibited borderline hypotension and was admitted to the hospital for rehydration, anti-emetic therapy, and observation. Additional laboratory studies were obtained including the blood smears shown at left. |
||
What organism most likely was the cause of this patient's febrile illness? |
|||
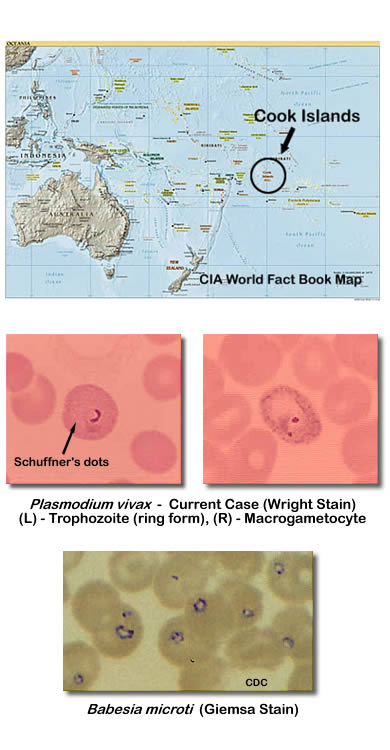 |
This patient had Plasmodium vivax malaria. What would have otherwise been a rather straight-forward diagnosis of malaria was made more difficult and confused by the fact that the CDC and WHO report that there is no risk of malaria in the Cook Islands (see map at left). This resulted in a delay in diagnosis. How this patient acquired malaria remains a mystery. The closest areas in which there is reported malaria risk are the Solomon Islands and Vanuatu over two thousand miles to the west. It is conceivable, but seemingly unlikely, that Tropical Cyclone "Trina" could have blown infected mosquitoes over such vast distances of the South Pacific. The patient's itinerary had involved non-stop flights Los Angeles to Rarotonga and return making infection enroute unlikely. It is also conceivable that he had become infected with malaria in Malawi two years previously. However, malaria acquired in Malawi would most likely be secondary to Plasmodium falciparum, a species lacking hypnozoite forms, making a late occurrence of clinical disease less likely. Finally, autochthonous transmission of malaria could have occurred as there are many immigrant farm workers in the Wenatchee Valley from countries where malaria is endemic. The diagnosis of Plasmodium vivax malaria was confirmed by the Washington State Health Department. Distinguishing the different species of malaria and distinguishing malaria from Babesia species requires epidemiologic information and skilled microscopy. Plasmodium vivax was diagnosed in this case as the red cells parasitized were macrocytes (reticulocytes) containing Schnuffer's dots. In contrast Plasmodium falciparum would parasitize red cells regardless of age. Babesia species (particularly Babesia WA-1) also had to be a consideration in this case particularly given the absence of reported malaria in the Cook Islands. Ring forms of Babesia (see images at left) can be very difficult to distinguish from those of Plasmodium falciparum. However, Babesia would not have other blood forms such as gametocytes as were seen in this case, and parasitization would not be confined to macrocytes. Because of local unfamiliarity with malaria and the uncertainty as to where the patient acquired his disease he was treated with quinine and doxycycline, and subsequently, primaquine. He experienced tinnitus and temporary hearing loss, both of which subsequently resolved. He suffered no further relapses. Babesiosis is an uncommon tickborne disease that occurs in the northeastern United States, the Midwest, and the West. The western variant is caused by Babesia WA-1. Illness can vary from subclinical to fulminant, malaria-like. Bartonella bacilliformis (see choices in original format) is a bacterium in which human infection can also have visible red cell inclusions. Bartonella bacilliformis is the agent of Oroya Fever and Verruga Peruana. Its occurrence is confined to areas of Peru, Columbia, and Ecuador. Ref: Malaria surveillance - United States, 2004, MMWR, Vol. 55, No. SS-4, May 26, 2006. |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||